The CEO had been listening to podcasts again. That's how the engineering lead at a Series A HealthTech startup described the moment everything went sideways. Leadership wanted to "overhaul the development process," convert product managers into "full-stack PMs" who could design, code, and test, and implement an eight-round interview process to rebuild the team from scratch. The startup had been stuck for years. The proposed solution? Fire everyone and start over based on frameworks from tech influencers who'd never shipped a HIPAA-compliant feature.
If you've felt that particular tension, watching product priorities pile up while internal capacity stays frozen, you're not alone. And the problem is bigger than any single dysfunctional leadership decision.
KEY TAKEAWAYS
Internal dev capacity blocks aren't just hiring problems, they're systemic misalignments between leadership expectations, technical debt, and realistic team capabilities.
HealthTech faces unique constraints: regulatory overhead, interoperability requirements, and security mandates consume 30-40% of development capacity before product work begins.
The $1.74 trillion IT services market exists because even well-funded teams can't scale internal capacity fast enough for AI and cloud demands.
Technical debt creates invisible capacity drains, one team went from 30% automation with 1,000+ weekly failures to 81.2% automation with fewer than 10 failures through focused refactoring.
The Hidden Capacity Crisis in HealthTech
Here's what the industry spending numbers reveal: global IT spending hit $5.74 trillion in 2025, with IT services alone representing $1.74 trillion, the largest single market segment. That's not companies building internal teams. That's companies admitting their internal teams can't keep up.
The Deloitte 2025 Technology Industry Outlook found that this 29% AI spending growth rate is straining internal dev teams and accelerating outsourcing across technology firms. In HealthTech specifically, where you're already burning capacity on HIPAA compliance, HL7 FHIR integrations, and FDA software validation, the pressure compounds exponentially.
The common belief was that IT services spending would slow as companies built internal AI dev teams. The reality? IT services remains the largest market because AI project overflow exceeds what internal capacity can absorb. You're not failing to hire well enough. The math simply doesn't work.
What Capacity Blocks Actually Look Like
One developer inherited what they described as "a tightly coupled mess of systems that broke constantly" at their new company. The automation system, critical infrastructure for their product, was stuck at 30% automation with over 1,000 failures per week. The automation was actually adding manual work, not reducing it.
"Taking a look under the hood unveiled a mess." A tightly coupled mess of systems that broke constantly.
u/kgthedev, Dev.to
This is what capacity blocks look like in practice. Not a lack of developers. Not insufficient budget. A system so compromised by technical debt that every hour of "productive" work generates two hours of cleanup. For HealthTech teams, multiply this by the regulatory documentation requirements, and you understand why roadmaps stall.
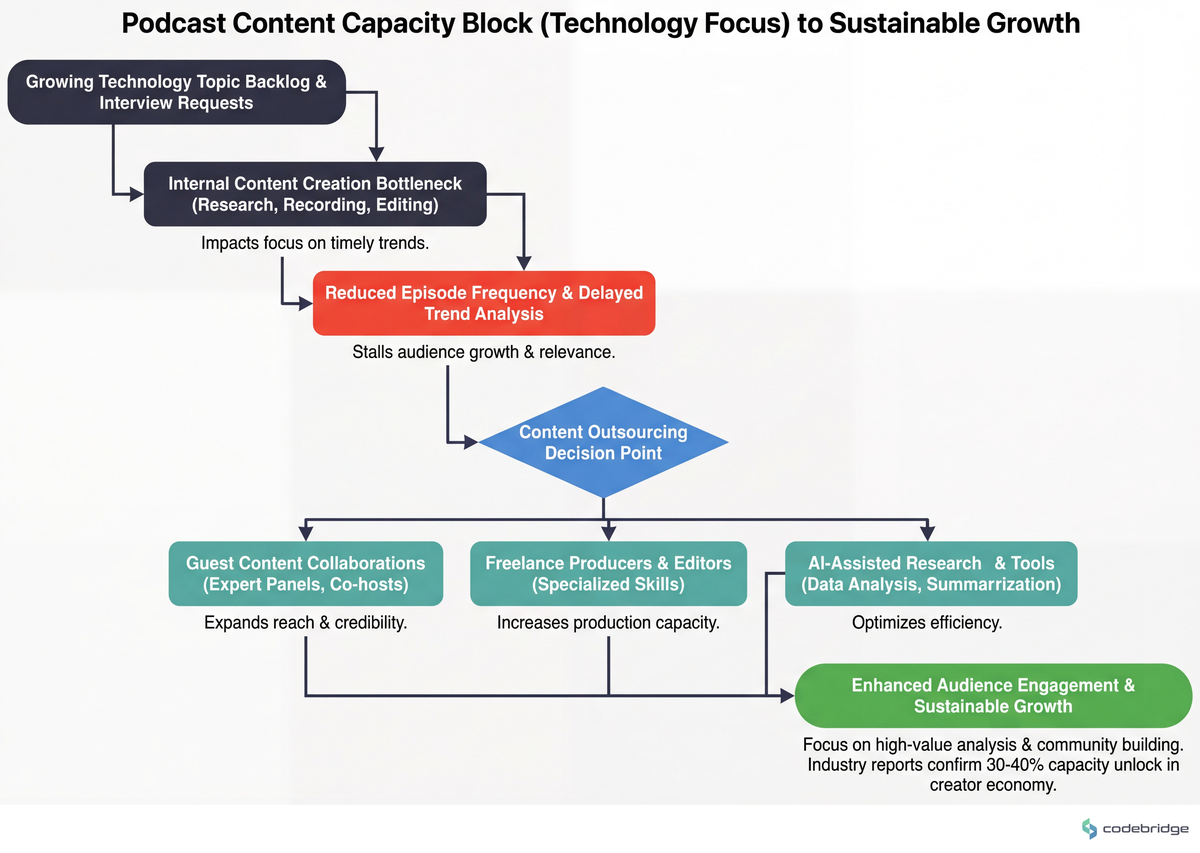
The pattern repeats across the industry. Consider how the major cloud providers have responded to their own capacity constraints. The following diagram illustrates how internal bottlenecks flow through to external partnerships:
Microsoft, facing internal capacity constraints for Azure and Copilot AI development, partnered with external IT services firms and invested heavily in AI-optimized data centers. The result: server spending contribution to data center growth exceeded 15% year-over-year, enabling a 14% software revenue surge. They didn't solve the capacity problem by hiring faster. They solved it by acknowledging the bottleneck and routing around it.
The Leadership Misalignment Problem
Back to that HealthTech startup with the podcast-influenced CEO. The engineering lead's observation cuts to the core issue:
"PMs cannot do EVERYONE'S jobs." It is impossible and actually borderline inhumane.
Anonymous Engineering Lead, Reddit r/ProductManagement
The CEO wanted "full-stack PMs" because some thought leader on a podcast made it sound efficient. What they actually needed was a realistic assessment of why their existing team, presumably hired with intention, couldn't ship product priorities. The answer almost certainly involved some combination of technical debt, unclear requirements, and regulatory overhead consuming invisible capacity.
This leadership misalignment creates a specific kind of block: the team knows what's wrong, but the proposed solutions from above don't address the actual constraints. You can't interview your way out of a codebase that fails 1,000 times per week.
When leadership seeks external validation (blogs, podcasts, conference talks) without operational context, proposed solutions rarely match actual constraints. The gap between "what sounds good" and "what works here" is where capacity blocks calcify.
The Pattern: What Successful HealthTech Teams Do Differently
The teams that break through capacity blocks share three characteristics that run counter to intuition.
First, they invest in infrastructure before features. This sounds backwards when your roadmap is backed up, but the data supports it. Data center systems spending grew 15.5% in 2025, faster than software's 14% growth, because AI hardware became the bottleneck. The common belief was that software growth would outpace infrastructure due to low dev costs. Reality proved otherwise. The teams that prioritized infrastructure unlocked capacity for everything else.
The developer who inherited that 30% automation disaster proved this at the team level. By focusing on refactoring the tightly coupled systems rather than pushing more features through broken pipelines, they achieved 81.2% automation with fewer than 10 weekly failures. That's not incremental improvement, it's capacity multiplication.
Second, they treat external capacity as a permanent part of the architecture, not a temporary fix. Google Cloud, facing explosive demand for GenAI infrastructure, expanded data center systems and IT services outsourcing for AI chip deployment. This contributed to $367 billion in global data center spend with 15.5% growth, powering their AI services. They didn't frame it as "we'll bring this in-house eventually." They designed for hybrid capacity from the start.
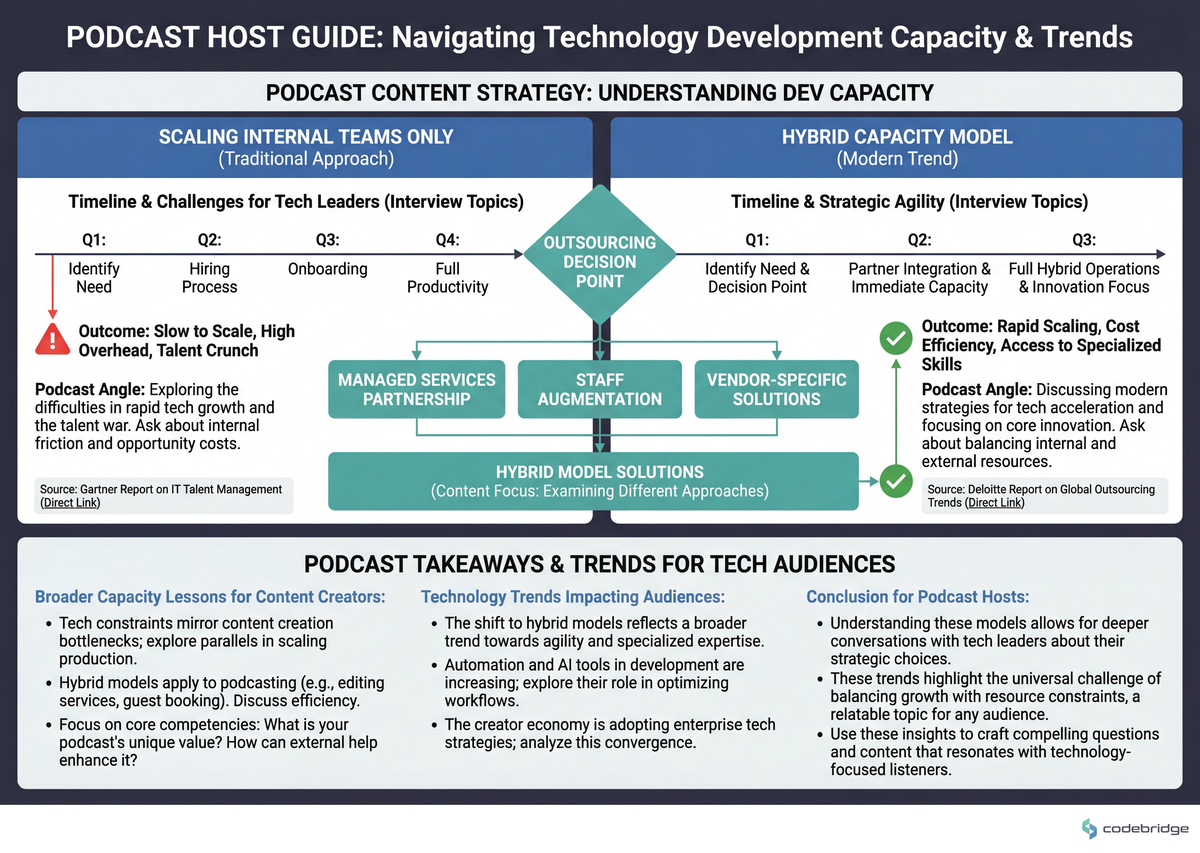
The comparison below shows how different approaches to capacity constraints play out over time:
Third, they separate capacity problems from capability problems. AWS, facing internal dev bottlenecks for cloud software amid 14% market growth, leveraged the IT services market through vendor partnerships and hybrid teams, achieving 9.4% year-over-year IT services growth while maintaining cloud dominance. The distinction matters: capability problems require training or hiring; capacity problems require load distribution.
A Framework for Diagnosing and Breaking Capacity Blocks
Based on the patterns from both the macro spending data and the individual team stories, here's a practical framework for HealthTech leaders facing capacity constraints:
1. Audit Your Invisible Capacity Drain
Before adding headcount or engaging external partners, quantify where capacity actually goes. The 30% automation / 1,000 failures scenario wasn't visible until someone looked under the hood. In HealthTech, common invisible drains include:
- Compliance documentation that's manually maintained rather than generated
- Integration testing that requires human verification due to brittle test suites
- Security reviews that restart from scratch on each release
- Interoperability testing with EHR systems that lacks automation
Track developer time for two sprints at task-level granularity. The ratio of "product work" to "maintenance work" reveals your true capacity.
2. Calculate Your Regulatory Overhead Percentage
HealthTech teams consistently underestimate how much capacity goes to non-feature work. A Series B digital therapeutics company (42-person team, React Native + Python backend on AWS) discovered they were spending 38% of engineering capacity on regulatory compliance activities that weren't tracked as such. They'd classified it as "documentation" and "testing", which it was, but the regulatory driver was invisible in their project management system.
Once visible, they could make informed decisions: automate compliance workflows, outsource specific compliance engineering, or accept the overhead and adjust roadmap expectations accordingly.
3. Distinguish Between Surge Capacity and Sustained Capacity Needs
The Information Technology market is projected to grow from $9.61 trillion in 2025 to $13.17 trillion by 2029 at 8.2% CAGR. That's not a temporary spike, it's structural demand growth driven by cloud computing and cybersecurity requirements. Your capacity strategy should reflect whether you're solving for a product launch surge or a permanent baseline increase.
| Capacity Need Type | Indicators | Appropriate Response |
|---|---|---|
| Surge (3-6 months) | Product launch, funding milestone, regulatory deadline | Staff augmentation, fixed-scope external teams |
| Sustained (12+ months) | Platform scaling, new product line, geographic expansion | Hybrid team model, infrastructure investment, process automation |
| Structural (permanent) | Ongoing compliance, security operations, data platform | Dedicated external partnerships, managed services |
4. Address Technical Debt as Capacity Investment
The 30% to 81.2% automation improvement wasn't a side project, it was the main project for a focused period. Frame technical debt reduction in capacity terms: "This refactoring will recover 15 developer-hours per week" is a business case. "We should clean up the codebase" is a wish.
5. Design for Hybrid Capacity from Day One
Gartner's VP Distinguished Analyst John David Lovelock projects the trajectory clearly:
"Our forecast projects that $500 billion will be added in spending every year For growth rates." With this in mind, IT spending should cross the $7 trillion mark in 2028.
John David Lovelock, VP Distinguished Analyst at Gartner
That $500 billion annual increase isn't going to internal teams. It's going to the hybrid capacity infrastructure that modern technology companies require. For HealthTech specifically, where specialized compliance and clinical knowledge intersect with software development, the hybrid model isn't a compromise, it's the architecture that matches reality.
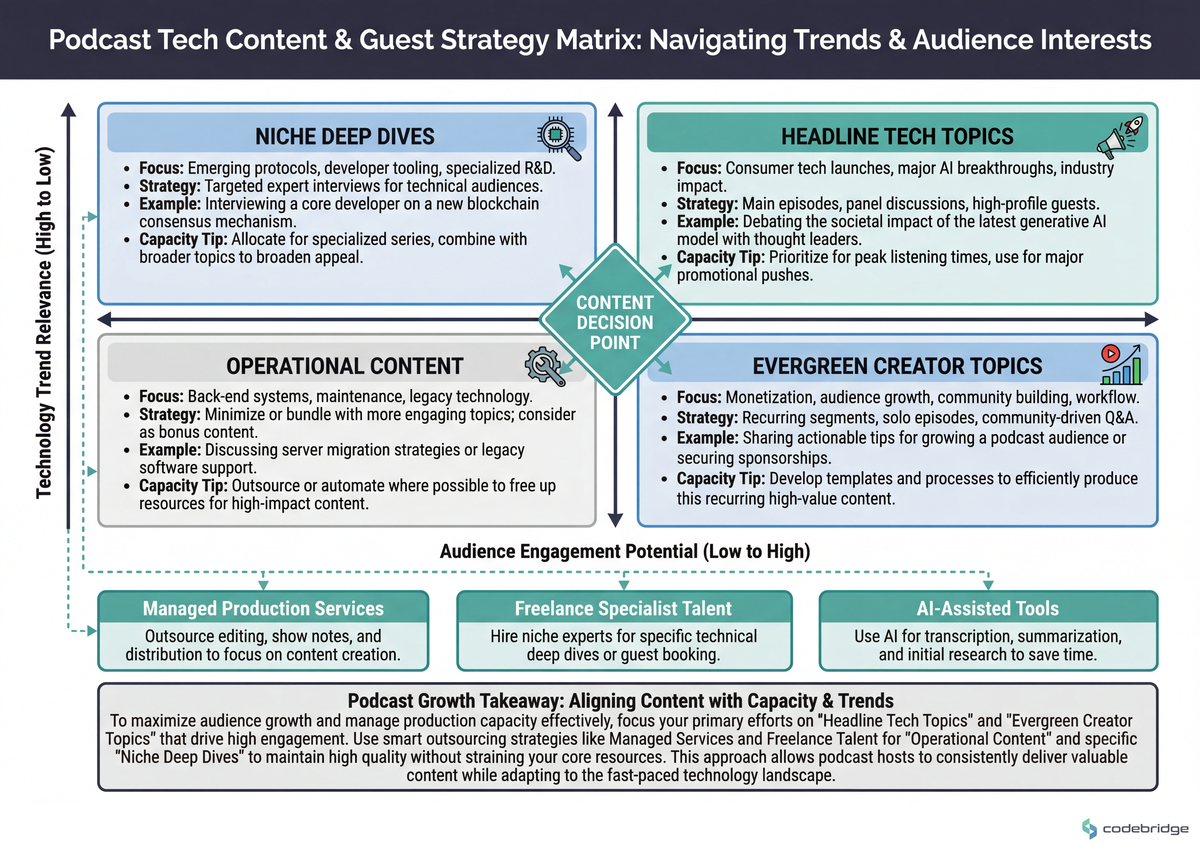
The following visualization shows how HealthTech teams can structure hybrid capacity across different work types:
The 2026 Landscape: What's Changing
Three trends are reshaping how HealthTech teams should think about capacity in the coming year:
AI-fueled IT services expansion is crossing new thresholds. Following 2025's $5.74 trillion spend, Gartner projects $7 trillion total IT spend by 2028 with 9%+ year-over-year growth. For HealthTech, this means AI capabilities that were experimental in 2024 are becoming table stakes, and the capacity to implement them isn't optional.
Data center systems hypergrowth for GenAI continues. Building on 2025's 15.5% surge, server sales are projected to hit $257 billion with the market tripling to $332 billion by 2028. HealthTech teams running AI diagnostic tools, clinical decision support, or patient engagement models need infrastructure capacity that most internal teams can't provision.
Sustainable IT practices are integrating with cloud/AI scaling.Research and Markets projects that climate tech integration with data center operations will drive the 8.2% IT market CAGR to $13.17 trillion by 2029. For HealthTech, this creates both pressure (sustainability reporting requirements) and opportunity (efficiency gains from optimized infrastructure).
Coming Back to the Waiting Room
That HealthTech startup with the podcast-influenced CEO? The engineering lead's frustration was valid, but the underlying problem wasn't the CEO's bad ideas, it was the absence of a shared framework for understanding why capacity was blocked in the first place. Without visibility into technical debt, regulatory overhead, and realistic team capabilities, leadership defaults to whatever framework sounds compelling on a podcast.
The path forward isn't firing everyone or implementing eight-round interviews. It's the unsexy work of auditing where capacity actually goes, distinguishing between capability and capacity problems, and designing for hybrid capacity that matches the structural reality of modern HealthTech development.
The teams that break through aren't the ones with the best hiring pipelines. They're the ones who stopped pretending that internal capacity alone could solve a problem that the entire $5.74 trillion IT industry has already acknowledged requires external partnerships.
Struggling to identify where your development capacity actually goes?
Schedule a capacity audit with our HealthTech engineering team.
Diagnostic Checklist: Signs Your HealthTech Team Has Capacity Blocks
Your sprint velocity has declined for 3+ consecutive sprints despite stable team size
More than 30% of developer time goes to maintenance, bug fixes, or "keeping the lights on" work
Compliance and regulatory documentation requires manual updates with each release
Your CI/CD pipeline has a failure rate above 10% on the main branch
Integration testing with EHR systems or external APIs requires manual verification steps
Leadership proposes team restructuring or process overhauls based on external frameworks without internal capacity data
Your roadmap has items that have been "next quarter" for more than two quarters
New feature development consistently takes 2x+ initial estimates due to unexpected dependencies
You've hired in the past 12 months but velocity hasn't increased proportionally













%20(1).jpg)
%20(1)%20(1)%20(1).jpg)





